Case discussion on 42 year old male with fever
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients' clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, and investigations, and come up with a diagnosis and treatment plan.
CASE DISCUSSION
42 year old male was brought with complaints of fever since 1 day with 1 episode of vomiting 1 day back.
History of presenting illness: The patient was apparently asymptomatic 1 day back when he developed fever which was incidious in onset, gradually progressive, high grade and relived on medication.
It was associated with chills and rigours and also burning micturition since 1 day.
However, he does not give history of any urgency or hesitancy in urinating.
He claims to have a decreased urine output since 4 days.
The 1 episode of vomiting, was around 1 pm the previous day. It was non bilious, non projectile, non blood stained with food as content.
No other complaints of any headache, neck stiffness, loose stools, abdominal pain
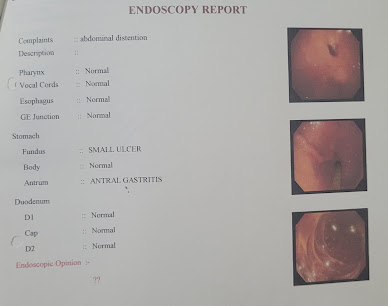
Past history: In Febuary 2023, patient developed abdominal tightness and chest discomfort and was hospitalized outside. Endoscopy was done there and he was diagnosed to have Antral gastritis.
1 month back patient presented with complaints of abdominal distension, pedal edema, lower back ache. He was hospitalized and found to have diabetes mellitus type 2 along with Chronic Kidney Disease. An MRI of lumbo sacral spine showed mild canal stenosis at L4-L5 and moderate canal stenosis at L3-L4 (early lumbar spondylosis with mild facetal arthropathy).
He is a k/c/o Hypertension since 4 years, on Tab. STAMLO BETA 0.5 mg PO/OD.
For his Type 2 DM, for 1 month, he has been taking Inj. HAI 8 U in the morning and 4 U in the evening s/c.
Not a k/c/o TB, asthma, epilepsy, CAD,CVA.
No major surgeries, no blood transfusions
O/E:
Patient is conscious, coherent and cooperative.
Pallor- Present
icterus- absent
cyanosis- absent
clubbing- absent
Lymphadenopathy - absent
Edema- Absent
Temp: 103.7° F
PR: 120 bpm
RR: 20 cpm
BP: 110/80 mmHg
SpO2: 98%
GRBS: 169 mg/dl
CVS: S1S2 +, no murmers
RS: BAE, NVBS
P/A: soft, non tender, no organomegaly, BS +
CNS: HMF intact, NFND
Provisional diagnosis: Pyrexia under evaluation, AKI on CKD secondary to Urosepsis with L3-L4 canal stenosis with Antral gastritis with type 2 Diabetes Mellitus
Investigations:
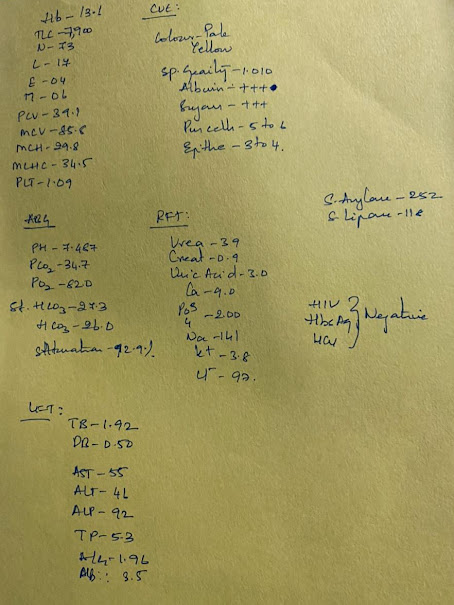
Reports on 7/6:
Plan:
1) Inj. NEOMOL 1 g iv/stat
2) IVF NS @75 ml/hr
3) Inj. HAI s/c
4) Inj. MONOCEF 1 mg iv/BD
5) Inj. PAN 40 mg iv/BD
Reports on 10/6:
S:
Fever spikes present at 12 pm yesterday
Stools passed
When asked, patient says he feels better
O:
Patient is conscious, coherent and cooperative
Afebrile to touch
PR- 80 bpm
RR- 19 cpm
BP- 120/80mmHg
CVS- S1 S2 present, no murmurs heard
RS-B/L air entry present, NVBS
PA- soft,NT, bowel sounds heard
CNS - GCS: E4V5M6
Tone:
Tone is Normal in right and left upper limbs.Tone increased in right and left lower limbs.
Power:
Right upper limbs: 5/5, Lower limbs: 5/5
Left upper limbs: 5/5, Lower limbs: 5/5
Reflexes:
Biceps: Rt: ++ Left: ++
Triceps: Rt: ++ Left: ++
Supinator: Rt: + Left: +
Knee jerk: Rt: ++ Left: ++
Ankle: Rt: + Left: +
Plantar: Rt: Extensor Left: Extensor
A
Complicated UTI (resolving) with CKD Stage 5 with L3-L4 Lumbar Stenosis ?Fluorosis or ? Myelofibrosis with Antral gastritis with Hypertension since 4 years and type 2 DM since 2 months
P
1) Inj. MONOCEF 1 g iv/BD
2)Tab. DOLO 650 mg PO/sos
3) Inj. HAI s/c TID
4) Monitoring vitals
On 12/6


.jpg)























Comments
Post a Comment