CASE DISCUSSION ON VIRAL PNEUMONIA SECONDARY TO COVID 19
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Neha Tipparaju
8th Semester, Roll no. 100
May 12, 2021
CASE OF VIRAL PNEUMONIA SECONDARY TO COVID 19
I've been given this case, in an attempt to understand the topic of "patient clinical data analysis" and to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations as well as to come up with a diagnosis and treatment plan.
All the information was obtained from the patient's relative, along with inputs from Dr. Praneeth Reddy sir (PG) and under the guidance of Dr. Rakesh Biswas sir.
My view of the case:
Chief Complaints
The patient, a 63 year old male patient, farmer by occupation and resident of Nalgonda, came with the complaints of:
Fever since 5 days
Cough with sputum since 5 days
Breathlessness even on rest since 4 days.
History of Presenting Illness
The patient was apparently alright 5 days back when he developed:
•Fever - Incidious in onset, mild (never reached above 100°F), continuous fever which was associated with chills and headache. It was not associated with any nausea and vomiting, burning micturition, chest or abdominal pain
•Cough with sputum- Productive cough with Scanty, mucoid sputum not blood stained or foul smelling. Cough is worse on lying down.
•4 days back, he developed Dyspnoea Grade 4 on MMRC dyspnea scale.
•Patient was taken to Hospital 1. When viral pneumonia was suspected on X ray, advised to come to Hospital 2 incase the need for Oxygen arises.
•sPO2 on admission: 75% Pulse rate: 110 bpm
•Patient was tested and declared Rapid Antigen Test COVID 19 positive and admitted.
History of Past Illness
•K/c/o Type 2 Diabetes Mellitus since 7 years on regular medication: Tab Metformin 500 mg OD
•K/c/o Chronic Kidney Disease since 2 years on conservative treatment.
•H/o Pulmonary Kochs: 7 years back (2014) for which he took 6 months of ATT.
•H/o Bronchial Asthma since 7 years (2014): Recurrent attacks during winter for which he takes measures like steam inhalations.
•H/o Chronic NSAID use: since 1991 for knee pain
• H/o Getting admitted to a Hospital in 2019 for B/L Pneumonia. Treated and Discharged.
• No h/o any cardiovascular anomalies, CVA.
Personal History
•Mixed diet is consumed. Appetite is normal but intake is supposedly reduced.
• Bowel and bladder are regular.
•Inadequate sleep due to breathlessness. Only 3-4 hours of sleep at night with frequent arousals.
• No known allergies
• Has stopped smoking and drinking since 35 years.
Family History
Not significant.
COVID contact
Examination
Patient was examined in a well lit room, after informed consent.
He was conscious, coherent and cooperative. Moderately built and nourished.
No pallor, icterus, cyanosis,clubbing,koilonychia,lymphadenopathy or generalized edema were observed.
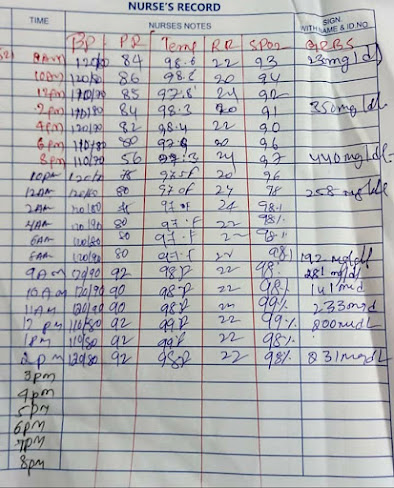
Vitals (admission) and Investigations ( as of 13/05/21)
Temp: 97. 2 degreesF
Respiratory Rate: 22 cpm
sPO2: 96% with 15lit of O2.
Systemic examination: CVS: S1, S2 heart sounds heard, no murmer.
Respiratory system: Bilateral air entry present
CNS: Intact
Abdomen: Soft and non tender, Bowel sounds heard no organomegaly.
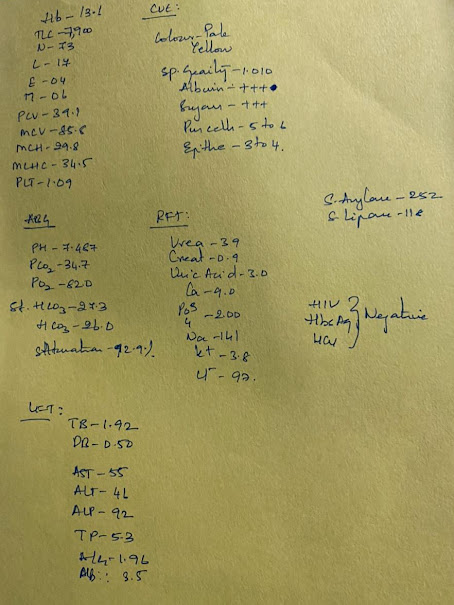
Urea: 72 mg/dL (elevated)
Creatinine: 2.1 mg/dL (elevated)
LDH: 600 IU/L (elevated)
CRP: 24 mg/dL (elevated)
D dimer: 690 ng/mL (elevated)
Investigations done
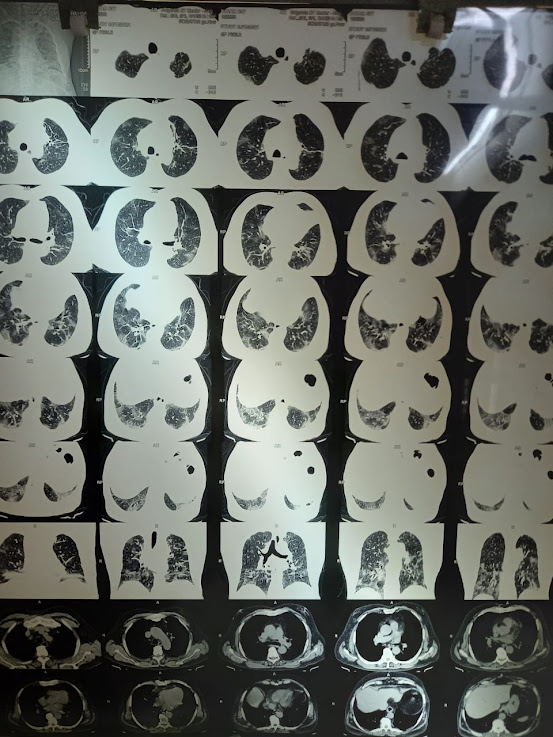
Chest x ray: diffuse areas of consolidation
HRCT-CORAD: 6
Vitals and Investigations (as of 14/05/21)
Temp: 98°F
Respiratory rate: 22 cpm
SPO2: 90% with 15 L of oxygen (fall compared to previous day)
CRP: 24 mg/dL ( same as previous day i.e elevated)
D dimer: 690 ng/mL (same as previous day i.e elevated)
Vitals and Investigations (as of 15/05/21)
Temp: 97.2° F
Respiratory rate: 22 cpm
Blood pressure: 110/70 mmHg
Pulse rate: 110 bpm
sPO2: 88% with 15L of O2 ( fall compared to previous day)
HRCT- CORAD: 6
Provisional Diagnosis
Severe pneumonia secondary to COVID of a k/c/o Diabetes, CKD, Bronchial Asthma and an old case of Pulmonary Koch.
Treatment Regimen ( 13/5, 14/5, 15/5)
1. Head elevation
2.O2 supplementation with 15 L/min
3.Neb with DUOLIN+BUDDCORT 6th hourly inj.
4.Dexamethasone 8mg IV tid
5.Inj. Clexane 60mg OD
6.Inj. Pan 40mg IV OD
7.Syp ascoryl LS 10ml TID
8.Tab PCM650 mg sos
9.Tab. Metformin 500mg OD
10.Inj pan 50mg OD
11.Inj.lasix 40mg iv BD
12.Tab.Nodosis 500mg OD
13.Tab. Mvt OD
14.Tab.Limcee OD
Vitals and Investigations ( as of 16/05/21)
Temp: 97.2°F
Respiratory rate: 24 cpm
Blood pressure: 110/70 mmHg
Pulse rate: 120 bpm
SP02: 60% with 15 L of O2 (fall compared to previous day)
Treatment: Intermittent CPAP started. SPO2 reached 90%
Medication continued as above
Vitals and Investigations (as of 17/05/21)
D dimers: 3540 ng/mL (Elevated from 690 ng/dL)
At 11 am, sPO2 was found to be 30% so patient was intubated.
As of 18/05/21








Comments
Post a Comment