Bimonthly Assignment for May 2021
Neha Tipparaju
Roll no. 100
I have been given the following cases to solve in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and to come up with a treatment plan.
This is a link to the questions of the Assignment:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to the assignment based on my comprehension of cases:
1) Pulmonology (10 marks)
A) Case e-log:
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The timeline of the patients symptoms can be summarised as follows:
From the above timeline line, it is clear that the main pathology of the patient is in her LUNGS. This can be in terms of the CHRONIC OBSTRUCTIVE PULMONARY DISEASE.
We know that:
The COPD in the patient might of been a result of long term inhalation of dust in the paddy fields which might have irritated the bronchiolar framework.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
• Head end elevation: improves end expiratory volume (https://pubmed.ncbi.nlm.nih.gov/24847096/)
•Intermittent BiPaP: ventilatory support (https://pubmed.ncbi.nlm.nih.gov/2686487/)
•Augmentin: antibiotics to prevent infection (penicillin) of bronchiectasis
•Lasix: Furosemide (loop diuretic) that activates Na+ K+ Cl- channels in nephron. To cure the pedal edema. (https://pubmed.ncbi.nlm.nih.gov/8800113/)
•Pantop: Proton pump inhibitor to decrease acid reflux
•Hydrocortisone: Steroid which is an anti-inflammatory.
•Ipavent: Ipratropium bromide- anticholinergic that will relax Bronchial muscles. (https://www.ncbi.nlm.nih.gov/books/NBK544261/)
3) What could be the causes for her current acute exacerbation?
Answer:
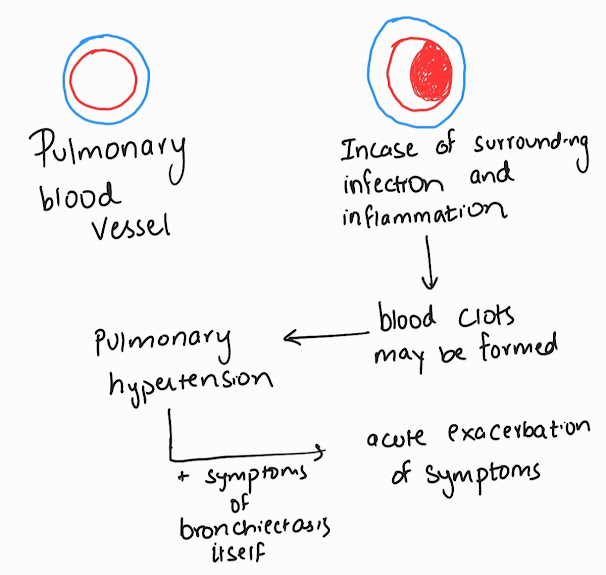
The exacerbation of the symptoms is most likely due to the infection of the lungs, the BRONCHIECTASIS that the patient has developed recently.
4) Could the ATT have affected her symptoms? If so how?
After some research, I have found a case report as shown:
Similarly, in our case as well, we can consider that the Antitubercular therapy may have worsened her heart failure.
This may have occurred due to the Antitubercular drugs, especially Rifampicin and Isoniazid, which are known to cause dilated cardiomyopathy, thus exacerbating her already present symptoms of right heart failure.
5) What could be the causes for her electrolyte imbalance?
Answer:
Her hyponatremia and hypochloremia are results of her Right Heart Failure and it's treatment. This can be because of:
• DIURETIC THERAPY: her use of Lasix may be leading to loss of electrolytes in Urine.
•Inappropriate water retention due to Vassopressin release.
• Failure of cell membrane ion pump.
2) Neurology (10 marks)
A) Case e-log:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The timeline of the patients symptoms can be summarised as follows:
From the above timeline, it is clear that the pathology is related to the patient's BRAIN. It can be related to the patient's dependence on Alcohol and withdrawal from it and can be secondary to damage of his kidneys.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
• Thiamine: to treat the deficiency (https://pubmed.ncbi.nlm.nih.gov/27818067/)
• Lorazepam: Enhances inhibitory effect of GABA, thereby preventing seizures (https://www.ncbi.nlm.nih.gov/books/NBK532890/)
• HAI (pre meal): Fast acting insulin to tackle the Hyperglycemia after a meal
• Lactulose (per oral): to treat constipation (https://www.ncbi.nlm.nih.gov/books/NBK536930/)
• For ulcer (daily dressing): promotes healing and prevents infection (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4121107/)
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
Answer:
The probable explanation for this can be:
The Acute Pre renal Kidney Injury in the patient that developed this time lead to uremic encephalopathy that explains the symptoms, along with the Wernicke's Encephalopathy associated thiamine deficiency as a consequence of chronic alcoholism.
4) What is the reason for giving thiamine in this patient?
Answer:
Hence, injection of 1 amp Thiamine in 100 mL, NS,TID is given to the patient to prevent worsening of symptoms.
5) What is the probable reason for kidney injury in this patient?
Answer:
Here, the state of Hyperglycemia (Diabetes) in the patient could have caused his AKI.
It could have also been augmented by chronic alcohol intake over the years, which may have damaged his kidneys.
Reference for this answer:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5898826/
6) What is the probable cause for the normocytic anemia?
Answer:
Normocytic normochromic anemia is characterized by normal size and colour of the Red Blood Cells in the blood, the defect being only decrease in number of RBC.
Blood Smear Picture of normocytic normochromic anemia (Picture taken from:https://www.researchgate.net/figure/Peripheral-blood-smear-examination-revealing-normocytic-normochromic-anemia-with_fig1_338738493)
In this case, the reason for the normocytic, normochromic anemia can be attributed to his Kidney Injury.
Kidney damaged--------≥ Decrease Erythropoietin production----≥ Decrease production of RBC by bone marrow.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Answer:
This can be explained as:
The injury to the foot may have been very trivial but due to the numbness and altered sensory input from the peripheral nerves ( as a result of chronic alcoholism as well as Diabetes), the injury was ignored and it aggrevated to an ulcer.
The injury to the foot may have been very trivial but due to the numbness and altered sensory input from the peripheral nerves ( as a result of chronic alcoholism as well as Diabetes), the injury was ignored and it aggrevated to an ulcer.
B) Case e-log:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
The timeline of symptoms can be summarised as follows:
From the timeline, it is clear that the patient's symptoms may be related to pathology in his Central Nervous System, particularly the BRAIN. The apparent aural symptoms can also be attributed to a central pathology.
The patient may have suffered with an ischaemic attack of the brain for which CHRONIC ALCOHOLISM and HYPERTENSION are risk factors.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
•Vertin: It is an antihistamine (antagonist for H3 receptors) to treat the aural symptoms like giddiness, tinnitus and hearing loss by reducing blood pressure in the stria vascularis (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2640000/)
•Zofer: An anti emetic, Odansetron that acts by blocking serotonin.
• Clopidogrel: Anti platelet agent to prevent blood clots (https://pubmed.ncbi.nlm.nih.gov/32568642/)
3) Did the patients history of denovo HTN contribute to his current condition?
Answer:
Hypertension is a very prevalent risk factor for Transient Ischemic Attacks and stroke. This can be explained as:
Possible arteries affected: Vertebral, Basilar or Posterior Cerebral arteries.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Answer:
•Reduced platelet aggregation
•Enhanced fibrinolysis
•Decreased plasma fibrinogen levels
All of which favour hemorrhagic conditions.
References:https://pubmed.ncbi.nlm.nih.gov/15330400/
C) Case e-log:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The timeline of symptoms in this patient can be summarised as:
From the above timeline, it is clear that the patient has and electrolyte imbalance that is causing her symptoms. The swelling of ankles and the weakness and paresis give clues that it could be HYPOKALEMIA.
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Answer:
Based on the finding that it was present since 10 years, we can consider Periodic Familial Hypokalemic Paralysis.
This is a genetic disorder where mutations affect the excitability of the muscle and it's ability to depolarize, resulting in recurrent episodes of paresis.
Alternate answers:
Considering various factors like:
•Female, age 45 years
•Symptoms like weakness, paresis.
•Evidence of hypokalemia
This can suggest a diagnosis of Primary Hyperaldosteronism.
Increased in aldosterone------≥ Retention of sodium-------≥ Excess excretion of potassium-------≥ pedal edema, weakness etc
However, a point against this is that the patient is normotensive.
Another point that can be considered is that the patient was using medication for her pedal edema for 8 months. If this medication was a diuretic, it can cause hypokalemia.
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
Answer:
The changes seen are:
•Flattening and invertion of T wave
•Q-T prolongation
• Visible U waves
•Mild S-T elevation
D) Case e-log:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Answer:
Post stroke seizures are common, particularly after an haemorrhagic stroke. The possible pathophysiology can be:
It is seen that Generalized Tonic Clonic Seizures are more commonly late onset. Late onset seizures are those which present after 6 to 12 months of the stroke attack and continue to recur. Recurrent seizures can be considered as Post stroke Epilepsy.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Answer:
The patient seems to suffering from an infection (Raised ALP and pleural effusion in lungs). This may have triggered the generalized tonic clonic seizure which lead to loss of consciousness. Abnormal increased activity in fronto-parietal association cortex and related subcortical structures is associated with loss of consciousness in generalized seizures.
E) Case e-log:
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Answer:
Ataxia is defined as the lack of muscle control or coordination of voluntary movements. In this patient, a change of gait was described.
The possible reasons for development of ataxia in this patient are:
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
Answer:
The binge drinking that occured 3 hours prior could have been responsible for an hemorrhagic stroke, in the form of an IC bleed.
In case of chronic alcoholism:
F) Case e-log:
1.Does the patient's history of road traffic accident have any role in his present condition?
Answer:
The patient may have had a Traumatic Brain Injury (TBI) then that would have gone undiagnosed. This state of TBI has a predisposition for ischaemic stroke as shown in this study: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC377
The study cohort included 1,173,353 total trauma subjects, 436,630 (37%) with TBI. The median duration of follow-up was 28 months (interquartile range 14–44), with a total of 11,229 (1%) ischemic strokes identified during this timeframe—1.1% in the TBI group and 0.9% in the non-TBI trauma group.
2.What are warning signs of CVA?
Answer:
The warning signs can be summarised as:
3.What is the drug rationale in CVA?
Answer:
The drugs given for a case of acute ischemic stroke are:
•t-PA: Tissue Plasminogen Activator-------≥ Activates Plasminogen which dissolves clots.
•Antiplatelet drugs: particularly Aspirin which prevents platelet aggregation by inhibiting cyclooxygenase enzyme.
In this patient the following drugs are being given:
* Aspirin
* Mannitol: to lower intra cranial pressure
* Atorvas: to control his lipid profile
4. Does his lipid profile has any role for his attack?
Answer:
The patient has a low level of High Density Lipoprotein (HDL). According to some studies, there is an inverse relation between the risk of stroke and HDL levels.
HDL has anti-atherosclerotic and anti-inflammatory properties and is an important component in preventing atherosclerosis.
Hence, it can be considered as a risk factor for atherogenic, ischaemic stroke.
G) Case e-log:
1)What is myelopathy hand?
Answer:
A characteristic dysfunction of the hand has been observed in various cervical spinal disorders when there is involvement of the spinal cord. There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
Conditions that can be considered if myelopathy hand is seen:
•Multiple sclerosis
•ALS
•Subacute combined degeneration
•Peripheral neuropathy
•Tumours or infection
2)What is finger escape ?
Answer:
Finger escape sign is also called Wartenberg's sign. It is the involuntary abduction of the little finger due to unopposed action of extensor digiti minimi muscle.
While this condition can be caused by various factors such as ulnar neuropathy or UMN disorder ( digiti quinti sign); it is considered Finger escape sign when it is caused by Cervical myelopathy for example, any mechanical compression of spinal cord.
3)What is Hoffman’s reflex?
Answer:
The steps involved to elicit this relex are:
•Position the subject’s relaxed hand ensuring dorsiflexion at the wrist and partial flexion of the fingers.
•Hold the subject's partially extended middle finger between your index and middle finger, ensuring you stabilize the proximal IP joint.
•Perform a sharp and forceful flick of your thumb, making contact with the nail of the subject’s middle finger.
•The subject's finger will flex immediately followed by relaxation.
•The presence of Hoffmann's sign is characterized by flexion and adduction of the thumb and flexion of the index finger.
A positive Hoffmann's sign is suggestive of corticospinal tract dysfunction localized to the cervical segments of the spinal cord.
Conditions such as multiple sclerosis, hyperthyroidism, and anxiety will also result in a positive sign.
Positive Hoffman sign: https://youtu.be/GJ-Q2ibYAHs
H) Case e-log:
1) What can be the cause of her condition ?
Answer:
The patient is having a Cerebral Venous Thrombosis (CVT) for which a common presenting feature is seizure. This can be classified as:
These seizures usually start as focal seizure which may get generalized.
Her headache and weakness can be a consequence of Iron Deficiency Anemia which is common in teenage girls (loss of blood through menstruation)
2) What are the risk factors for cortical vein thrombosis?
Answer:
These include:
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Answer:
Seizures occur because of imbalances in the electrical activity in the brain. This imbalance may spontaneously be corrected which terminate the seizure episode and lead to a seizure free period. (Doubtful answer)
4)What drug was used in suspicion of cortical venous sinus thrombosis?
Answer:
The patient was started on Tab Acitrom 2 mg/PO/OD which is an oral coumarinic anticoagulant.
It acts by inhibiting the action of Vitamin K epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting.
3) Cardiology
A) Case e-log:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Answer:
Ejection fraction (EF) is a measurement, expressed as a percentage, of how much blood the left ventricle pumps out with each contraction.
Normal EF is between 55% to 70%
Heart failure can be classified as follows:
2.Why haven't we done pericardiocenetis in this pateint?
Answer:
Pericardiocentesis is indicated only when the pericardial effusion is not resolving on its own. In this case, there is a decrease in fluid around the heart (resolving : 2.07cms effusion at the time of admission -1.4mm at the time of discharge) and hence pericardiocentesis is not done.
3.What are the risk factors for development of heart failure in the patient?
Answer:
They are:
4.What could be the cause for hypotension in this patient?
Answer:
The patient is severely anemic. Anemia is a risk factor for hypotension, both systolic and diastolic as it leads to hypovolemia. Hence the anemia could have lead to his hypotension.
B) Case e-log:
1.What are the possible causes for heart failure in this patient?
Answer:
The possible risk factors are:
2.what is the reason for anaemia in this case?
Answer:
Anemia of inflammation, also called anemia of chronic disease or ACD, is a type of anemia that affects people who have conditions that cause inflammation, such as infections, autoimmune diseases, cancer, and like in this case, chronic kidney disease (CKD).
It is a form of normocytic, normochromic, hypoproliferative anemia.
The reason is attributed to decreased production of erythropoietin by the damaged kidneys.
Hence:
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
Answer:
The patient has peripheral neuropathy due to his uncontrolled Diabetes. Hence a trivial injury would have been ignored and it progresses to an ulcer stage.
Peripheral Vascular disease caused decreased blood flow to the limbs.
Diabetes and Hypertension are also states with low immunity which could have contributed to infection in his legs.
4. What sequence of stages of diabetes has been noted in this patient?
Answer:
C) Case e-log:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The timeline can be summarised as:
Hence, the patient's symptoms seem to have a cardiac origin which may have now affected his kidneys. Hypertension may be one reason attributed to this.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Answer:
Cardiorenal syndrome (CRS) is an umbrella term used in the medical field that defines disorders of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction of the other.
It can be classified as follows:
In this case, the patient seems to have Type 4 CRS.
3) What are the risk factors for atherosclerosis in this patient?
Answer:
The risk factors in this patient are:
• Hypertension
•Diabetes detected
• Alcohol history (?)
4) Why was the patient asked to get those APTT, INR tests for review?
Answer:
To predict the clot formation and subsequent attacks of CVA or ischaemia that might occur in this patient. To monitor whether the anticoagulants are working.
D) Case e-log:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The timeline can be summarised as:
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
The various interventions are:
• Glimi: sulfonylurea that increase insulin release to reduce blood sugar. (https://www.japi.org/q2c45494/efficacy-of-the-modern-su-glimepiride-in-reducing-hyperglycemia-in-t2dm)
• Telma: Angiotensin Receptor Blocker that lowers blood pressure. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2937316/)
3) What are the indications and contraindications for PCI?
Answer:
Indications:
•Acute ST-elevation myocardial infarction (STEMI)
•Non–ST-elevation acute coronary syndrome (NSTE-ACS)
•Unstable angina
•Stable angina
•Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
•High risk stress test findings.
Contraindications:
•Intolerance for oral antiplatelets long-term
•Absence of cardiac surgery backup
•Hypercoagulable state
•High-grade chronic kidney disease
•Chronic total occlusion of SVG
•An artery with a diameter of <1.5 mm
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Answer:
The possible risks of PCI are:
•Bleeding
•Blood vessel damage
•Allergic reaction to the contrast dye used
•Arrhythmias
•Need for emergency coronary artery bypass grafting
To minimize these risks, it is better to do PCI in those who actually need it
Overtesting and overdiagnosis: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6135119/
E) Case e-log:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The timeline can be summarised as follows:
Diagnosed as Hypertensive and Diabetic----------≥ Developed Chest pain 3 days back.
The Chest pain and the risk factors such as hypertension and diabetes point to a Cardiac pathology.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
The various interventions are:
• HAI: Fast acting insulin to tackle the Hyperglycemia after a meal.
•Angioplasty and stent: to open blocked vessels (https://pubmed.ncbi.nlm.nih.gov/9462572/)
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Answer:
The procedure was necessary in order to repurfuse the patient's heart. It was successful in the fact that the patient improved after the procedure.
F) Case e-log:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Answer not known
(To my knowledge SOB worsens in cardiac patients given fluids as there is already a fluid overload in the body)
2.What is the rationale of using torsemide in this patient?
Answer:
Torsemide is a diuretic used to treat high blood pressure and condition of excess fluid retention in the body due to heart failure. This will help to relieve his symptom of SOB.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Answer:
The antibiotic was administered to treat the UTI as the patient did complain of whitish discharge in the urine which may be a sign of infection.
The patient also has a risk for further infection as he is using a Foley's catheter so the antibiotic can be prophylactic also.
4) Gastroenterology (and Pulmonology)
A) Case e-log:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The timeline can be summarised as follows:
Based on this timeline, it is clear that the patient has a gastrointestinal pathology probably triggered by Alcohol intake.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Answer:
•Meropenam, Metrogyl, Amikacin: antibiotics to control infection (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5392851/)
•Octreotide: Somatostatin long acting analogue to decrease exocrine pancreas secretions (https://pubmed.ncbi.nlm.nih.gov/10207228/)
•Thiamine: to supplement the deficiency in alcoholics
B) Case e-log:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
Answer:
The patient has a pleural effusion which is causing his dyspnea.
Two main causes of pleural effusion are:
• Transdiaphragmatic lymphatic blockage leading to increased permiability.
• Pancreaticopleural fistulae secondary to leak and disruption of the pancreatic duct or pseudocyst caused by an episode of acute pancreatitis.
These changes are mediated by inflammatory cytokines.
Some examples:
2) Name possible reasons why the patient has developed a state of hyperglycemia.
Answer:
The possible reasons can be:
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Answer:
The patient is a chronic alcoholic due to which his liver could have been affected, elevating his LFTs.
•AST level is more than twice that of ALT
• Elevated levels of Gamma Glutamyl Transferase
4) What is the line of treatment in this patient?
Answer:
C) Case e-log:
1) What is the most probable diagnosis in this patient?
Answer:
The patient is suffering with a Ruptured Liver Abscess, Intraperitoneal hematoma and Grade 3 Renal parenchymal Disease of the right kidney.
2) What was the cause of her death?
Answer:
Mortality after an Emergency Laparotomy is high, due to complications. In this case, the patient developed shortness of breath (either due to anaesthesia or mucus build up in her lungs?) and expired.
3) Does her NSAID abuse have something to do with her condition? How?
Answer:
NSAIDs, by inhibiting cyclooxygenase enzyme, decrease the amount of cytoprotective prostaglandins and may cause kidney disease.
5) Nephrology (and Urology)
A) Case e-log:
1) . What could be the reason for his SOB ?
Answer:
The reason for his SOB can be:
2. Why does he have intermittent episodes of drowsiness ?
Answer:
The reason for his drowsiness can be:
3. Why did he complaint of fleshy mass like passage in his urine?
Answer:
The patient had Pyuria: pus cells in the urine, so he felt like a white mass was passing in his urine.
4. What are the complications of TURP that he may have had?
Answer:
B) Case e-log:
1.Why is the child excessively hyperactive without much of social etiquettes ?
Answer:
There are many reasons for a child in the developmental age to present with features like being excessively hyperactive, impulsive, not having proper social etiquettes as is expected of his age, too active to pay any attention at school, talk so fast that even comprehending sentences becomes quite difficult.
The most common reason we can think of is:
Attention deficit hyperactivity disorder (ADHD) which is a mental health disorder that can cause above-normal levels of hyperactive and impulsive behaviors. People with ADHD may also have trouble focusing their attention on a single task or sitting still for long periods of time.
2. Why doesn't the child have the excessive urge of urination at night time?
Doubtful answer
This may be attributed to any psychosomatic disorder or undiagnosed anxiety disorder that is causing the frequent urination in the child.
3. How would you want to manage the patient to relieve him of his symptoms?
Answer:
Proper counselling of the child and the mother should be done.
If he is confirmed to have ADHD, behavioural therapies and medication like stimulants, atomoxetine, alpha-2 adrenergic receptor agonists, and sometimes antidepressants can be tried.
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology)
A) Case e-log:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
Answer:
The findings of:
•Difficulty in swallowing
•Finding on barium swallow
•Finding on Endoscopy
• Suspicion: HIV-----≥ Candidial infection-------≥ Tracheo esophageal fistula
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Answer:
Immune reconstitution inflammatory syndrome (IRIS) describes a collection of inflammatory disorders associated with paradoxical worsening of preexisting infectious processes following the initiation of antiretroviral therapy (ART) in HIV-infected individuals.
Current theories concerning the pathogenesis of the syndrome involve a combination of:
•underlying antigenic burden
•degree of immune restoration following Highly active antiretroviral therapy (HAART)
•host genetic susceptibility
A cohort analysis shows that 17-23% of people on ART develop IRIS syndrome. The chances are more in this patient as she is also on anti-TB medication.
( Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221202/)
With careful monitoring, this syndrome is usually self limiting.
7) Infectious disease and Hepatology:
A) Case e-log:
1. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? (since 30 years - 1 bottle per day)
Answer:
Alcohol causing liver damage:
Some studies show that amoebic liver abscess (ALA) cases occur in alcohol drinkers. In experimental studies, the presence of 'iron' potentiates the in-vitro growth of Entamoeba histolytica (E. histolytica), and is also known to increase its in-vivo invasiveness in animal infections. Chronic alcoholism increases the hepatic iron deposition.
(Reference: https://pubmed.ncbi.nlm.nih.gov/12924485/)
3. Is liver abscess more common in right lobe ?
Answer:
Since the liver receives its blood circulation from the systemic and portal circulations, it is more susceptible to getting infections and abscesses from the bloodstream. As the right lobe recieves more blood supply, it is the more common site for formation of liver abscess.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
Answer:
The indications are:
•Large abscess more than 6cms
•Left lobe abscess
•Abscess failure to respond to drugs
• Any large abscess which is impending to rupture
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology)
A) Case e-log:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The timeline of symptoms can be summarised as:
Based on the timeline the patient has an infectious etiology that has affected his eye, nasal cavity as well as neurologically also. The diabetes may have contributed to the immunocompromised nature, leading to infection.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Answer:
•Itraconazole: antifungal that acts by inhibiting the fungal cytochrome P-450 dependent enzyme lanosterol 14-α-demethylase. (https://pubmed.ncbi.nlm.nih.gov/1324238/)
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Answer:
The possible reasons are:
• Increased use of steroids
•Prevalence of diseases like Diabetes, liver and kidney diseases
•Use of immunosuppressive drugs for autoimmune diseases
• Prolonged hospital stay, using mechanical ventilators
• Poor hygienic environment.
9) Infectious Disease (Covid 19)
Master chart: https://1drv.ms/b/s!Atq20WQGNFJWqeMe3jRXZ4Bl8axZ9A
10) Experimental medical learning
Making this e-log helped us maintain a competency of history taking skills needed while dealing with patients that we feared might be lost due to staying away from the hospital environment. While the online classes help us with our theoretical knowledge, this e-log based case presentation has enabled us to expand our clinical and practical mindset where we are able to freely interact with each other and our professors to put forth our ideas as well as clear our doubts. Grateful and thankful for the opportunity.



















































Comments
Post a Comment