CASE DISCUSSION ON 25 YEAR OLD MALE WITH EPIGASTRIC PAIN
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Neha Tipparaju
8th Semester, Roll no. 100
May 20, 2021
CASE OF 25 YEAR OLD MAN, WITH SEVERE EPIGASTRIC PAIN
I've been given this case, in an attempt to understand the topic of "patient clinical data analysis" and to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations as well as to come up with a diagnosis and treatment plan.
All the information was obtained from the patient's relative, along with inputs from Dr. Vilasith sir, Dr. Raveen sir and under the guidance of Dr. Rakesh Biswas sir.
My view of the case:
Chief Complaints:
A 25 year old man,daily wage worker and tractor driver by occupation, presented with:
•Severe abdominal pain since 4 days
•One episode of vomiting 2 hours before presenting to hospital
•Shortness of breath on walking since 2 hours.
History of Presenting illness:
Patient was fine, 4 days back, when he developed:
Abdominal pain which was Sudden in onset, gradually progressing, in the epigastric region, not migrating or radiating backwards, aggrevated on lying down and relieved in sitting position.
He also gives history of an episode of vomiting, 2 hours back which was non projectile, not blood stained, non bilious and not associated with any vertigo, fever, loose stools etc.
He also had Dyspnea of Grade 3 on MMRC dyspnea scale.
No h/o: Facial puffiness, pedal edema, fever, burning micturition, frothy urine, hematuria
No h/o polyuria, polydipsia, polyphagia and nocturnal enuresis
The patient is known to abuse alcohol. His last drink was 4 days prior to the onset of symptoms.
Past history
There were no similar complaints in the past
The patient is not a k/c/o Diabetes, Hypertension, Asthma, Tuberculosis or Epilepsy
No known drug allergies
Personal history
Diet: Mixed
Appetite: Normal
Bowel and bladder: Regular
Sleep: Reduced due to pain
Addictions: Alcohol intake since 4 years which was weekly once or twice.
However, since last 2 months, daily consumption of 2 Litres of Toddy.
Family history
Not significant.
Examination
Patient was examined in a well lit room, after informed consent.
He was conscious, coherent and cooperative. Patient looked malnourished and dehydrated.
No pallor
No icterus
No cyanosis
No clubbing
No koilonychia
No lymphadenopathy
No generalized edema
No pedal edema was observed.
JVP was not seen to be raised.
Vitals (admission)
BP: 130/80 mm of Hg
PR: 116 bpm (high)
Respiratory Rate: 24 cpm (high)
Tempature: 98.4°F
GRBS: 242 mg/dL (elevated)
SPO2: 90% on RA (Less than normal)
Systemic examination:
CVS: S1 and S2 heart sounds heard. No murmers
Respiratory system:Bilateral air entry is present, Bilateral decreased breath sounds at IAA and ISA
Per Abdomen: Soft, Tenderness around umbilical and epigastric regions
No organomegaly
No guarding
No rigidity
No rebound tenderness
No shifting dullness
Bowel Sounds heard
CNS: Intact
Investigations
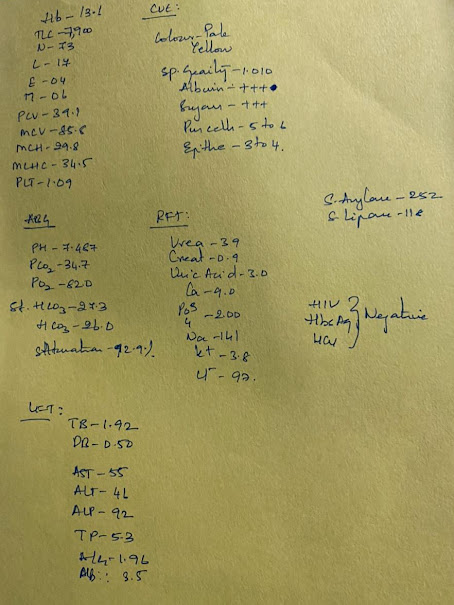
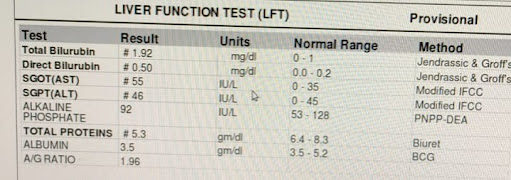
CBP, CUE, ABG, LFT, RFT as shown:
Noteworthy points:
•Albumin and Sugar in Urine
•Saturation: 92.8% (decreased)
• Serum amylase: 252 U/L (elevated)
•Serum lipase: 118 IU/L (elevated)
X ray of chest, as shown:
Pleural effusion: obliterated costophrenic angles
USG report, as shown:
Noteworthy points:
•Altered echotexture of head of pancreas
•Grade 1 Fatty Liver
•Minimal Ascites
ECG, as shown:
Differential Diagnosis
1) Acute Pancreatitis (Points favouring: Tenderness, Raised amylase, lipase levels, USG finding)
2) Acute Cholecystitis (Points against: Pain is not radiating, No Murphy's sign USG findings)
3) Perforated peptic ulcer (Points against: No abdominal rigidity or shifting dullness)
Provisional Diagnosis:
Acute pancreatitis.
Denovo Type 2 Diabetes Mellitus (?)
Plan of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
Related Questions
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
2) Name the possible reasons why this patient has developed a state of hyperglycemia.
3) Reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver Disease?
4) What is the line of treatment in this patient?















Comments
Post a Comment