Case discussion on 65 year old female with giddiness
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients' clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, and investigations, and come up with a diagnosis and treatment plan.
CASE DISCUSSION:
65 year old female, resident of Shakapuram village in Nalgonda district and a housewife came on 15/4/23 with complaints of giddiness since 4 months.
History of presenting illness:
Patient was apparently asymptomatic 4 months back when she started to develop episodes of giddiness, which led to a fall at home leaving her unconscious for a few seconds. She had 2 more similar episodes 3 months back and the most recent episode, which was 2 months ago caused her a fracture in her right hand.
The episodes of giddiness were associated with loss of consciousness for around 3-5 seconds. There was no h/o of any ENT bleed, any seizures, vomitings, headache or thinking/memory disturbances after the falls. She regained consciousness in about 5 seconds and did not lose it again at any time after the fall, in between the episodes.
She also complains of giddiness while lying down, which lasts for 2 minutes and is relived automatically. Postural variation +. For these symptoms,the patient has been using medication since 2 months. Tab. PROCHLORPERAZINE 5 mg PO/OD
No c/o nausea, vomiting, loose stools, fever, cough or cold
No c/o motion sickness,chest pain, palpitations or shortness of breath
No h/o postural drop, ataxia
No h/o any major trauma to head
Past history:
There were no similar complaints in the past.
Patient is a k/c/o Hypertension since 30 years, on regular medication of Tab. ATENOLOL 50 mg PO/OD.
Not a k/c/o Diabetes mellitus, asthma, TB,epilepsy, CAD, arrhythmia, thyroid dysfunction.
H/o hysterectomy done 40 years back
H/o Bilateral knee replacement 10 years back.
H/o 1 PRBC blood transfusion done 10 years back
Personal history:
Takes mixed diet,
Normal appetite
Bowel and bladder are regular
Sleep adequate
No Addictions
No Allergies
No Significant family history.
General Examination:
Patient is conscious, coherent and cooperative.
On examination, there are no signs of pallor, icterus, cyanosis, clubbing, koilonychia, generalized edema or lymphadenopathy.
Sensory examination:
Crude touch, pain ,temp, fine touch, joint position, proprioception are normal in all dermatomes in upper and lower limbs.
Cerebellum examination:
Able to do finger nose test.
No dysdiadokinesia
No rebound tenderness
No ataxia
Rombergs test: Negative
No fall/swaying with patient's eyes closed. Romberg test: NegativeAutonomic Nervous System:
No postural hypotension
No bladder and bowel incontinence
No sweating abnormalities
Meningeal signs:
No meningal signs like Brudzinski or Kernig sign were positive
Gait: Normal
Provisional diagnosis:
Giddiness under Evaluation
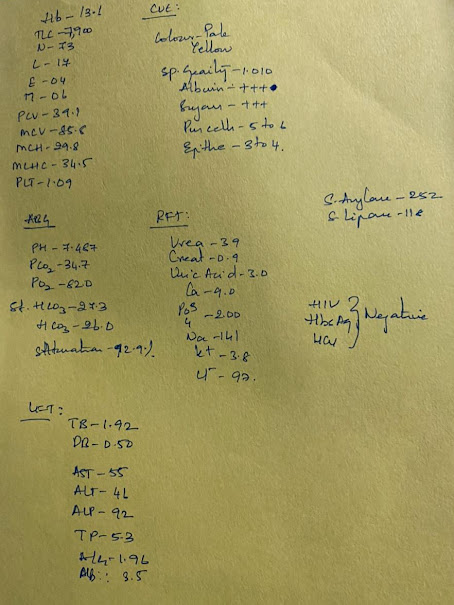
Investigations (15/4/23):
Plan of care:
1) Tab ATENOLOL 50 mg PO/OD
2) Tab PROCHLORPERAZINE 5 mg PO/OD










Comments
Post a Comment