Case of 80 year old male with upper limb and lower limb weakness
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Neha Tipparaju
Roll no. 100
Case of an 80 year old male with Upper and Lower limb weakness
My case is of an 80 year old male, who was a shepherd by occupation and a resident of Miryalguda, came to the OPD with chief complaints of neck pain and weakness of upper and lower limbs since 3 days.
Timeline of events and history of presenting illness:
5 years ago: Patient was a shepherd. He used to leave at 6 am and come back at around 4 pm. He stopped working on the advice of his family as he was getting tired very easily and had frequent falls in the field.
Since then, he stays at home all day and was able to look after himself in terms of brushing, bathing, feeding etc.
3 days ago (1/2/2022): Patient had his dinner around 8 pm and retired to bed. He then suddenly fell off the bed and complained of neck pain and inability to use both his upper and lower limbs. He was taken to the local RMP who checked his blood pressure and told him he was hypertensive. Unknown medication was given.
The weakness was not a/w loss of consciousness, slurring of speech, drooping of mouth, seizures, tongue bite or frothing of mouth, difficulty in swallowing.
No complaints of any headache, vomitings, chest pain, palpitations and syncopal attacks.
No shortness of breath, orthopnea, paroxysmal nocturnal dyspnea, abdominal pain or burning micturition.
Since 2 days, the patient has slurring of speech and non productive cough.
Past history:
No similar episodes in the past.
Not a known case of diabetes mellitus, asthma, epilepsy, coronary artery disease.
No surgical or drug history
Personal history:
They take a mixed diet, appetite is normal, bowel and bladder are regular, sleep is adequate. He was an occasional toddy drinker, 90 mL during festivals. Stopped 5 years back. Does not smoke. No known allergies.
Family history:
No similar complaints in the family
Patient is examined in a well lit room after obtaining informed consent. She is conscious, coherent and cooperative, well oriented to time, place and personn, moderately built and nourished.
On General Examination:
Pallor: Present
Icterus, cyanosis, clubbing, koilonychia, generalized lymphadenopathy or edema are not observed.
Vitals:
Temp.- Afebrile
BP- 190/100 mmHg
PR- 92 bpm
RR- 21 cpm
SpO2- 96%
GRBS- 144 mg/dL
INVESTIGATIONS:-
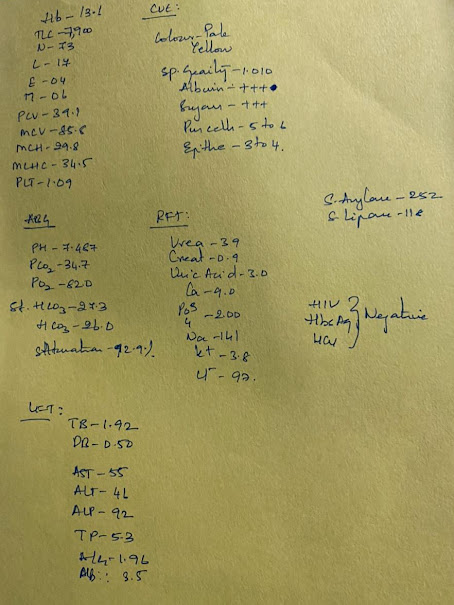
HEMOGRAM-
HB:- 8.3GM/DL
TC:- 5,300
N/L/E /M :- 95/ 02/01/02
PCV :- 25.6
MCV- 80.5
MCH:- 26.1
MCHC:- 32.4
RBC :- 3.18
PLATELETS:- 4.72
NORMOCYTIC NORMOCHROMIC ANEMIA WITH NEUTROPHILIC LEUCOCYTOSIS.
COMPLETE URINE EXAMINATION:-
PUS CELLS- 3-4
EPITHELIAL CELLS - 2-3
ALBUMIN:- TRACE (2.8)
SUGARS:- NIL
RBS- 162MG/DL
FBS:- 144MG/DL
PLBS:- 126MG/DL
LFT:-
TB:- 0.55
DB:- 0.18
AST:- 19
ALT:- 10
ALP:- 135
TOTAL PROTEIN:- 5.7
A/ G RATIO:- 0.96
RFT:-
BLOOD UREA -52
SERUM CREATININE - 0.9
Na:- 137
K:- 5.8
Cl:- 102
HBA1C:- 6.6 %
FASTING LIPID PROFILE:-
TOTAL CHOLESTROL:- 112MG/DL
TRIGLYCERIDES:- 174 MG/DL
HDL CHOLESTEROL:- 30MG/DL
LDL CHOLESTROL:- 89 MG/DL
VLDL:- 35MG/DL
MRI:
IMPRESSION:-
1) MODERATE TO SEVERE CERVICAL SPONDYLOSIS AT MULTILEVEL C2-C3 , C3-C4 , C4-C5 & C5-C6 LEVEL WITH COMPRESSIVE MYELOPATHY CHANGES AND SPINAL CANAL STENOSIS
2) NEURAL IMPRINGEMENT AT C4-C5 , C5-C6 LEVELS.
Xrays:
USG report:
Bilateral Grade 2 Renal Parenchymal Disease with Simple cortical cyst.
Chest: Mild pleural effusion on right
Mild pleural effusion on left with Consolidation in peripheral lung parenchyma
Provisional diagnosis:
? Compressive myelopathy
Treatment:
1) IV FLUIDS @75 ml/hr
2) CERVICAL HARD COLLAR
3) TAB AMLONG 5MG PO/OD
4) TAB PAN 40MG PO/OD
5) TAB ZOFER 4MG PO/ SOS
6) BP/ PR/ RR / TEMP CHARTING
7) STRICT IPO CHARTING
8) INJ OPTINEURON 1 AMP IN 100ML NS / IV / OD
Pleural tap was advised.












Comments
Post a Comment