Case of a 78 year old male with altered sensorium
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Neha Tipparaju
Roll no. 100
Case of a 78 year old male with altered sensorium
My case is of a 78 year old male, resident of Ramanpet, who used to be a farmer by occupation.
The patient was brought to casuality with altered sensorium after a fall.
(Timeline of events)
5 years back, the patient had a mild fever for which he was taken to a hospital. On screening there, he was found to be Type 2 diabetic and started on medication Tab. Metformin 500mg OD.
3 years back, he was found to be hypertensive and started on Tab Atenolol 50 mg OD.
He took medications regularly and was mostly assymptomatic ( blurring of vision, was adviced spectacles: presbyopia?)
25 days back he had a thorn prick injury to his left foot, below the second toe. He ignored this and it grew to ulcerate.
10 days back, the left foot was surgically debrided and dressed
History of presenting illness:
At 6 pm on 8/1/22, The patient had fallen from the bed due to loss of balance,his head hitting the corner of the table and hence sustained an injury on his left frontal region, near the left eyebrow.
He was fine for an hour after the fall. However, after 1 hour, he suddenly stopped responding to his family's questions, had breathlessness and palpitations, tremors,anxiety, was sweating profusely and was drowsy.
He was brought to the casuality. His vitals showed:
Heart rate: 115 BPM
Respiratory rate: 22 cycles/ min
Blood pressure: 210/ 120 mmHg
Temperature: Afebrile
SPO2: 78%
Random blood sugar: 40 mg/ dl
• On examination, His Glasgow coma score was 11.
Eye opening was spontaneous (4)
He was confused, did not response verbally (4)
Was in a flexed posture (3)
• Inspiratory crepitations were heard in all the lung fields.
He was given O2 supplementation at 15 mL/hour and 25% dextrose i.v stat. He recovered and began to respond to commands.
He sustained an injury to right 5th toe at night while walking to the washroom and this was appropriately dressed.
Presently, the patient is not complaining of any nausea, sweating, tremors, palpitations or headache.
He is not complaining of any chest pain, orthopnea, PND, swelling of limbs or any cough
No complaints of change in urinary frequency (decrease or increase), no fever, suprapubic pain or burning micturition
No complaints of blurring of vision, weakness for moving limbs, bowel and bladder incontinence
No fever, headache, vomiting or neck rigidity
Past history:
There were no similar episodes in the past. K/c/o Diabetes since 5 years and hypertension since 3 years. Not a k/c/o asthma, tuberculosis, epilepsy, coronary artery disease or cerebrovascular accidents.
No surgeries in the past
Drugs: Tab. Metformin 500 mg OD for 5 years
Tab. Atenolol 50 mg OD for 3 years.
Personal history: The patient takes a mixed diet. Appetite is reduced and bowel and bladder are regular. He gets an adequate amount of sleep. No known allergies.
He used to smoke beedi everyday for 30 years, before he stopped 10 years back.
He occassionally drinks 60ml of toddy.
Family history: no relevant family history
General Examination: Patient is examined in a well lit room after obtaining informed consent. He is conscious, coherent and cooperative, thinly built and nourished.
On examination:
Pallor: Moderate
Icterus, cyanosis, clubbing, koilonychia, generalized lymphadenopathy or edema are not observed.
Vitals:
Heart rate: 90 BPM
Respiratory rate: 20 cycles per min
Blood pressure: 130/90 mmHg
Temperature: 98.6 °F
SPO2: 98%
RBS: 118 mg/dl
Systemic Examination:
Central Nervous System:
CNS:
Higher mental functions:
Oriented to time,place,person
Memory : recent, remote intact
Speech: normal, understandable
No delusions or hallucinations
Cranial nerves:
1- not tested
2- binocular vision: normal
colour vision:normal
3,4,6- No restriction of movement of eye
5-normal( muscles of mastication+sensations of face) No jaw jerk
7-Normal, wrinking of forehead seen, able to blow up cheeks
8- Normal hearing
9,10,11,12-normal. Gag reflex is normal.
Motor examination:
Tone -normal
Power
-4/5 in b/l lowerlimbs
-4/5 in upper limbs
Reflexes :
Biceps:b/l:2+
Triceps:2+
Supinator 2+
Knee: not elicited (pain of the wounds)
Ankle: not elicited
Plantars: not elicted
Sensory examination:
crude touch, pain ,temp, fine touch, joint position, proprioception are normal in all dermatomes in upper limbs.
Pain sensation seemed to be decreased in lower limbs, particularly the foot.
Cerebellum examination:
Able to do finger nose test.
No dysdiadokinesia
No rebound tenderness
Autonomic Nervous System:
No postural hypotension
No bladder and bowel incontinence
No sweating abnormalities
Meningeal signs:
No meningal signs like Brudzinski or Kernig sign were positive
Gait: walk with limp due to wounds.
CVS: S1 S2+ no murmurs heard.
Respiratory system- Bilateral air entry+ ,normal vesicular breath sounds-heard.
Abdominal: Soft, non tender, no distension, umbilicus is central and inverted,no scars, no sinuses, hernial orifices free.
Provisional diagnosis:
Episode of altered sensorium secondary to hypoglycemia
K/c/o Diabetes and hypertension
Investigations:
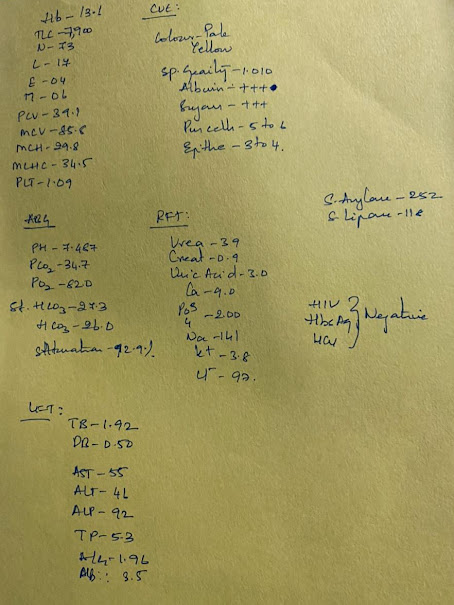
Significant: Hemoglobin: 10.1 gm/dl
MCV: 70 fl
MCHC: 34.4
Platelet count: 1.3 lakh
Microcytic hypochromic anemia with relative thrombocytopenia.
No features suggestive of liver or kidney dysfunction.
ECG:
Management:
SOAP notes:
Subjective:
Episode of hypoglycemia
No nausea, vomiting, fever
Ulcer on left foot. Wound on right 5th toe
Objective:
Pt is C\C\C
Afebrile
Bp: 130/90 mmHg
HR: 90 BPM
RR: 17 cycles/min
GRBS: 118 mg/dl
CNS: intact
CVS: S1S2 +
RS: BAE+
P/A: Soft, non- tender
Assessment: K/c/o Diabetes and Hypertension, microcytic hypochromic anemia
Plan:
On 8/1 : Inj 25% Dextrose i.v stat
5% Dextrose at 50 ml/hour (increase or decrease according to GRBS)
Presently: Inj Piptaz 4.5 g i.v
BP, GRBS monitoring
Chest xray, CT brain and fundoscopy advised.
•What triggered his hypoglycemia?
Age? Decreased physiological response to falling blood sugar.
Hypoglycemia unawareness
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499525/
https://pubmed.ncbi.nlm.nih.gov/30724638/
•What is the reason for his microcytic anemia?
•Is there a relation between anemia and diabetes?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166192/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4658398/
These studies have shown that diabetes, associated with increase in Inflammatory mediators like IL-1 and IL-6, affects the production of RBC.
(Can this be considered as Anemia of Chronic disease?)
Diabetes can contribute to iron deficiency through reduced iron absorption, gastrointestinal bleeding and the complications like nephropathy.
:








Comments
Post a Comment