This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Neha Tipparaju
Roll no. 100
Case of 45 year old lady with lower back pain
My case is of a 45 year old lady, agricultural worker by occupation and resident of Nalgonda, who came with the complaints of:
Lower back pain since 1 year.
Weakness of right lower limb since 2 days
History of presenting illness:
Patient was apparently assymptomatic 1 year back when she developed a lower back ache. This pain was incidious in onset gradually progressive for a duration of 1 year.
The pain is a dragging type, which radiates along the right limb and is aggrevated on continuous standing or walking and relieved on rest and medication of NSAIDs, which she has been taking for 6 months, on the advice of an orthopaedician. He directed her to get a Lumbar MRI and advised her for surgery, which she did not follow through due to personal issues in the family.
No history of any fall or trauma
Patient had difficulty in passing stools (constipation) since 1 month for which the patient went to the nearby doctor 2 days back. She was put on Syp. Lactulose and after 1 day, the patient had 5 episodes of watery stools for 1 day, 2 episodes of vomitings for 1 day which subsided now.
The patient is also complaining of generalized weakness since 2 days
Presently the patient is not complaining of any fever, cough, headache, diarrhoea, vomitings, burning micturition or suprapubic pain.
Past history:
No similar complaints in the past
Not known to be having Diabetes mellitus, hypertension, tuberculosis, asthma, epilepsy, coronary artery disease or cerebro vascular accidents.
Previous surgeries/ interventions: Hysterectomy 10 yrs back
ECSL for Right Renal stones 6 years back,
Left Cataract Surgery 6 yrs back.
Using NDAIDs for the last 6 months for back pain.
Personal history:
P3L3
Diet- mixed
Appetite- Reduced due to pain
Sleep- Adequate
Bowel and bladder movements- Regular
No known allergies
No addictions
Family history: Not significant
General Examination:
Patient is examined in a well lit room after obtaining informed consent. She is conscious, coherent and cooperative, well oriented to time, place and personn, moderately built and nourished.
On examination:
Pallor: Mild
Icterus, cyanosis, clubbing, koilonychia, generalized lymphadenopathy or edema are not observed.
Vitals:
Temp.- Afebrile
BP- 110/70 mmHg
PR- 100 bpm
RR- 12 cpm
SpO2- 98%
GRBS- 138 mg/dL
Systemic Examination
CNS:
Higher mental functions:
Oriented to time,place,person
Memory : recent, remote intact
Speech: normal, understandable
No delusions or hallucinations
Cranial nerves:
1- not tested
2- binocular vision: normal
colour vision:normal
3,4,6- No restriction of movement of eye
5-normal( muscles of mastication+sensations of face) No jaw jerk
7-Normal, wrinking of forehead seen, able to blow up cheeks
8- Normal hearing
9,10,11,12-normal. Gag reflex is normal.
Motor examination:
Tone -normal
Power
-4/5 in right lower limbs
5/5 in left lower limb and upper limbs
Reflexes :
Biceps:b/l:2+
Triceps:2+
Supinator 2+
Knee: Right: 1+
Left: 3+
Ankle: Right: 1+
Left: 2+
Plantars: Decreased response on right side
Sensory examination:
Crude touch, pain ,temp, fine touch, joint position, proprioception are normal in all dermatomes in upper limbs.
Crude touch and pain are decreased on all dermatomes of right lower limb.
Cerebellum examination:
Able to do finger nose test.
No dysdiadokinesia
No rebound tenderness
Autonomic Nervous System:
No postural hypotension
No bladder and bowel incontinence
No sweating abnormalities
Meningeal signs:
No meningal signs like Brudzinski or Kernig sign were positive
Gait: did not walk due to pain
CVS: S1 S2+ no murmurs heard.
Respiratory system- Bilateral air entry+ ,normal vesicular breath sounds-heard.
Abdominal: Soft, non tender, no distension, umbilicus is central and inverted,no scars, no sinuses, hernial orifices free.
Investigations:
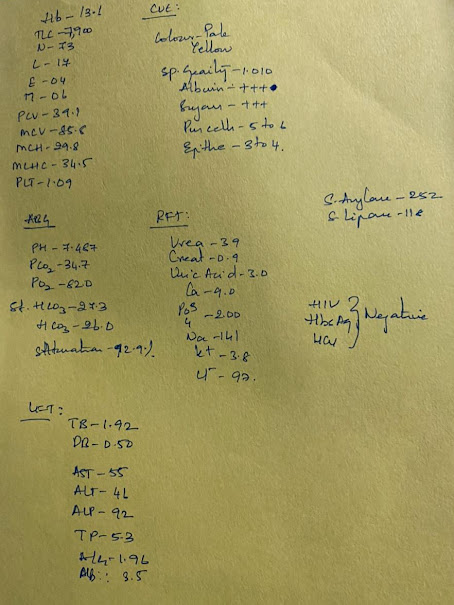
Significant findings: Microcytic hypochromic anemia, Low platelets, elevated creatinine and urea
Ultrasonography:
X ray:
MRI :
(On orthopaedic advice)
PROVISIONAL DIAGNOSIS:
AKI secondary to ?analgesic neuropathy
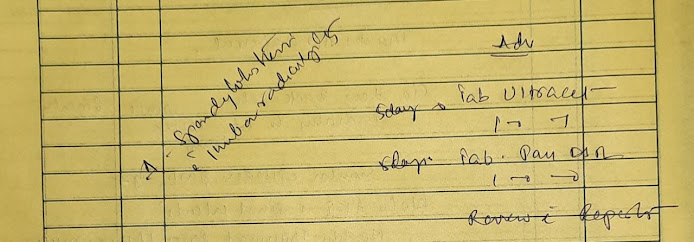
TREATMENT GIVEN:
1. IV Fluids NS and RL @ UO+50 ml/h
2. Inj. Optineuron 1 amp in 100 ml NS
3. Inj. PANTOP 40 mg IV OD
4. Inj. Lasix 20 mg IV BD (if sBP>110 mmHg)
5. Inj. Neomol 100 ml IV SOS (if temp>101 F)
6. Tab. PCM 500 mg PO SOS
7. GRBS - 6th hrly
8. I/O Charting
9. Monitor vitals 4th hrly
Orthopaedic referral:
Nephrology referral:


















Comments
Post a Comment