CASE DISCUSSION ON 16 YEAR OLD MALE WITH DENGUE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Neha Tipparaju
9th Semester, Roll no. 100
Case of 16 year old male with Dengue fever
I've been given this case, in an attempt to understand the topic of "patient clinical data analysis" and to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations as well as to come up with a diagnosis and treatment plan.
All the information was obtained from the patient's relative, under the guidance of Dr. Rakesh Biswas sir.
My view of the case:
Chief complaints:
A 16 year old male, resident of Nalgonda, was bought to the casuality, complaining of:
Fever since 5 days
Pain abdomen since 5 days
2 episodes of vomitings
His vitals on admission in the casuality (on 26/10/21) were:
Heart rate: 103 BPM
Respiratory rate: 18 cpm
Blood pressure: 90/50 mmHg
SPO2: 98% Room air
Presently, the patient is complaining of itching all over the body, especially on the palms and soles.
History of presenting illness:
Patient was apparently assymptomatic 5 days back when he developed a fever which was incidious in onset, intermittent, low grade and not associated with any headache, diarrhoea, chills or rigour.
He also complained of pain abdomen, diffusely present in all quadrants, intermittent, squeezing type of pain, not radiating or migrating and relieving on medication.
On the evening of 26th, the patient had 2 episodes of vomiting which was non bilious, non blood stained, non projectile. It was preceded by nausea.
The patient did not complain of any burning micturition, rash, hematemesis, melaena, epistaxia, hemoptysis or hematuria.
Patient has developed an itching sensation all over the body, which is not relieving on medication.
Past History:
No similar complaints in the past.
He is not a k/c/o Diabetes mellitus, hypertension, tuberculosis, asthma, heart disease
No relevant surgical or drug history
Personal history:
Diet is mixed
Appetite is normal
Bowel and bladder are regular
Sleep is adequate
No known allergies or addictions
Family history:
Not significant
General Examination:
The patient is examined in the sitting position, in a well lit room after taking informed consent.
He is conscious, coherent, cooperative, well oriented to time, place and person.
Moderately built and nourished. On examination for signs:
No pallor
No icterus
No cyanosis
No clubbing
No koilonychia
No lymphadenopathy
No generalized edema
No pedal edema was observed.
JVP was not seen to be raised.
Vitals:
BP: 100/70 mm of Hg
PR: 64 bpm
Respiratory Rate: 21 cpm
Tempature: 98.7°F
Systemic examination:
CVS: S1, S2 heart sounds heard, no murmer
Respiratory system: Bilateral air entry present
CNS: Intact
Abdomen: Soft and non tender, Bowel sounds heard no organomegaly
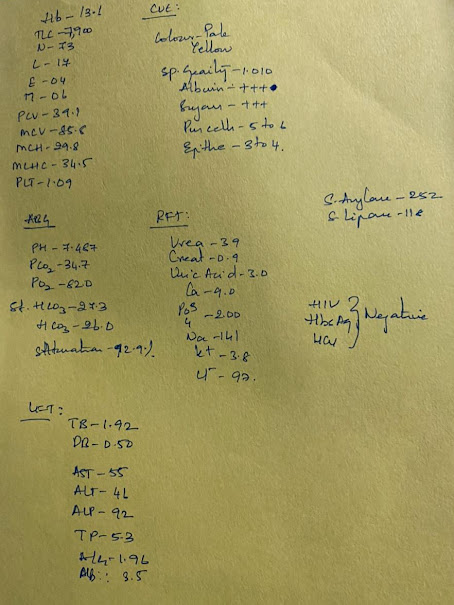
Investigations: (27/10)
As of 28/10






Comments
Post a Comment