Case discussion on 50 year old female with generalized weakness and abdominal discomfort
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients' clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, and investigations, and come up with a diagnosis and treatment plan.
CASE DISCUSSION
50 year old female, resident of Nalgonda and housewife came to OPD on 19/4/23 with c/o Generalised weakness since 2 days, 2 episodes of giddiness since 1 day and abdominal pain with chest discomfort since 1 day.
History of presenting illness:
The patient was apparently asymptomatic 2 days back and then she started feeling weak and was not able to perform her daily tasks as well as she used to. The sequence of events are as follows:
1 day back, she felt giddy and weak in the morning which was relieved on taking (?) medication.
She had another similar episode in the evening which did not relieve with the same medication. She went to a local RMP who found her to be hypotensive and started her on I.v Fluids.
At 3:00 am (approximately 6 hours later) the patient felt extremely weak and went to a government hospital. Her BP there was found to be 193/120 and she was treated with T. VERTIN and T. AMLODIPINE.
She persistently felt weak and was anxious about her health and so was brought to our hospital.
She also c/o abdominal discomfort since 1 day. She has a feeling of abdominal distension along with burning sensation in chest which is relieved on eating
The 2 episodes of giddiness were associated with diffuse headache, nausea and tremors. No c/o vomiting, postural drop, aggravation with head movements or any hearing disturbance
No c/o any fever, loose stools, vomiting, burning micturition, cough or cold
No c/o palpitations or SOB
Past history:
Patient has been having the symptoms of abdominal discomfort with burning sensation on and off since 1 year
Recently, she had similar complaints 1 month back, which were relieved on medication. (Syr. MUCAINEGEL 10 ml TID; Tab. PAN 40 mg PO/OD/BBF; Tab. CLONAFIT BETA)
Used antihypertensive medication 1 month back for 5 days and then stopped.
Not a k/c/o Diabetes Mellitus, asthma, TB, epilepsy, CVA,CAD, thyroid dysfunction
1 lower segment C section done 21 years back i/v/o abnormal presentation of baby. Tubectomised
No h/o any blood transfusions
Personal history:
Takes mixed diet,
Normal appetite
Bowel and bladder are regular
Sleep adequate
Occasionally drinks toddy or beer (once in a month)
No Allergies
No Significant family history.
General Examination:
Patient is conscious, coherent and cooperative.
On examination,
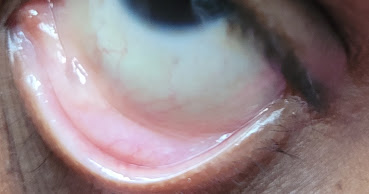
Pallor +
No signs of icterus, cyanosis, clubbing, koilonychia, generalized edema or lymphadenopathy
VITALS:
Temp:97.8°F
B.P:160/110 mmhg
P.R: 77 bpm
R.R:20 cpm
Systemic examination:
CVS: S1S2 heard, no murmers
RS: BAE +, NVBS heard, no added sounds
P/A: On Inspection, abdomen is obese with central umbilicus and all quadrants moving equally with respiration. No visible sinuses or pulsations.
On palpation, there is no local rise of temperature or tenderness, no palpable masses, hernial orifices were free and organs were not palpated due to obese abdominal wall.
Bowel sounds were heard.
CNS: Patient is oriented to time,place and person. Cranial nerves are intact. Sensations felt over b/l limbs. Muscle tone is maintained in b/l limbs. Power is 4+ in b/l limbs. B/l Biceps, Triceps, knee, ankle Reflexes are grade 2+, supinator is 1+ and plantar reflex shows flexion.
No neck stiffness, vomitings
No ataxia, nystagmus, finger nose incoordination, dysdiadochokinesia
Romberg sign is negative
Provisional diagnosis:
Acid Peptic Disease under evaluation with ?Denovo HTN
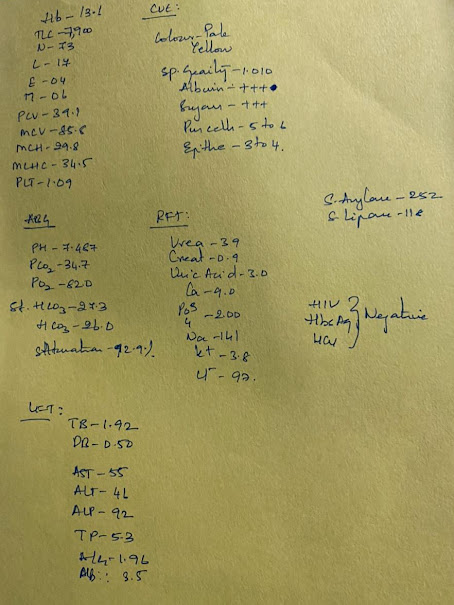
Investigations (19/4/23):















Comments
Post a Comment