Case discussion on 65 year male patient with fever and cough
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Long case
1701006128
Case discussion of 65 year male with Fever and Cough
A 65 year old male patient, a former daily wage labourer and resident of Cherlapally came with the chief complaints of:
Cough with sputum since 1 month
Shortness of breath since 5 days
Abdominal pain since 5 days
Fever since 5 days
Timeline of events and History of Presenting illness
Patient was a daily wage labourer who did not have any significant morbidity, ever requiring hospitalization
2 years back, he stopped going to work due to tiredness
1 year back, he had similar complaints of fever and cough with sputum. On visiting a local Registered Medical Practitioner (RMP) he was diagnosed with having Pulmonary tuberculosis and started on Anti tubercular therapy.
Patient took treatment for 2 months and then discontinued as he felt that he recovered.
1 month back, the patient developed cough and went to a local RMP who started him on some medication that the patient says is the same as before, therefore, Anti TB medication that he is continuing to take.
5 days back, the patient's cough was aggrevated in a way that he would get bouts of wet cough along with shortness of breath,abdominal pain and fever
He went to a local hospital. On investigation was found to be Diabetic (de novo). Was refered to our hospital for treatment.
Cough has been present for a duration of 1 month. It is wet cough with thick, dark red sputum of mucoid consistency. The sputum in amount can fill half cup and was sometimes blood stained. No aggrevating or relieving factors
Shortness of breath has been present for a period of 5 days.Gradually progressive He is not able to walk because of it, putting that at MMRC grade 4. It was aggrevated on sitting up . Relived on lying in right lateral decubitus position
He also has been complaining of abdominal pain since 5 days. The pain was sudden in onset and progressive. It is diffuse, persistent type of pain with no referal, radiation or migration,aggrevating or relieving factors.
Patient has been febrile for the past 5 days. Incidious in onset and progressive, continuous with no diurnal variation. It was not associated with chills and rigours, vomiting, diarrhoea or headache.
Patient also has burning micturition since 5 days. He did not complain of any decreased urine output nor any increased frequency of micturition, did not complain of poor stream, nocturia or urgency. No pedal edema. Pain was not radiating nor any referral. No aggrevating or relieving factors.
Patient also has weight loss. He weighed 60kg a year back but now weighs 45kg.
Patient did not give any complaints of vomiting, diarrhoea, constipation, abdominal distension, headache.
Past history:
Similar complaints 1 year back as mentioned.
He is a known case of Tuberculosis. De novo Diabetes Mellitus.
Not a known case of hypertension, asthma, epilepsy, coronary artery disease or any bleeding disorders
No surgeries, blood transfusions in the past
Drug history: Anti tubercular drugs
Personal history:
He takes mixed diet
Appetite is reduced due to abdominal pain
Bowel and bladder are regular
Sleep is inadequate
No allergies
Chronic smoker: 3 packs of beedi per day for 50 years (Smoking index= 3×9×50= 1350)
Chronic intake of alcohol: 90 ml per day for 50 years
Family history: No similar complaints in the family. No history of tuberculosis in the family
General Examination:
Patient is examined in supine position in a well lit room, after taking informed consent.
He is breathless and clearly using accessory muscles for respiration.
Patient is conscious, coherent and cooperative. Poorly built and poorly nourished (emaciated)
On examination there were no signs of pallor, icterus, cyanosis, clubbing, koilonychia, generalized lymphadenopathy, generalized edema or pedal edema.
His vitals were:
Temperature: 102° F
Pulse rate: 112 bpm
Respiration: 18 cpm
Blood pressure: 130/90 mmHg
GRBS: 173 mg%
Systemic Examination of Lower Respiratory system:
Patient is observed in supine position.
Inspection
Abdomino thoracic type of breathing
Trachea is central
Chest looks to be barrel shaped. It is symmetrical.
Movements are slightly decreased on right side
No scars, sinuses or visible pulsations
No nasal flaring
Suprasternal and supraclavicular notching is present
Apical impulse not seen
Palpation
No local rise of temperature
No tenderness
Inspectory findings are confirmed: Trachea is central, movements decreased on right side.
Anteroposterior diameter of chest >Transverse diameter of chest
No crowding of ribs, rachitic/scorbutic rosary
Apex beat felt in 5th intercostal space
Tactile vocal fremitus:
Supraclavicular: Decreased on right, felt on left
Infraclavicular: Decreased on right, felt on left
Inframammary: Decreased on right, felt on left
Axillary: Decreased on right, felt on left
Infraaxillary: Decreased on right, felt on left
Suprascapular
Interscapular: Not examined
Intrascapular
Percussion
Supraclavicular: Stony dull on right, Resonant on left
Infraclavicular: Stony dull on right, Resonant on left
Inframammary: Stony dull on right, Resonant on left
Axillary: Stony dull on right, Resonant on left
Infraaxillary: Stony dull on right, Resonant on left
Suprascapular
Interscapular: Not percussed
Intrascapular
Auscultation
Breath sounds were decreased on right side in all areas.
Vocal resonance was decreased on right side in all areas.
Adventitious sounds: Not heard
Examination of other systems:
Cardiovascular system: S1 S2 heard, no murmers
Central Nervous system: Intact
Abdominal examination: Guarding, rigidity and tenderness present
Provisional diagnosis:
Right sided Pleural effusion secondary to community acquired Pneumonia (Parapneumonic effusion)
De novo Diabetes Mellitus
Differential diagnosis:
Reactivation of tuberculosis: Tubercular Pleural effusion
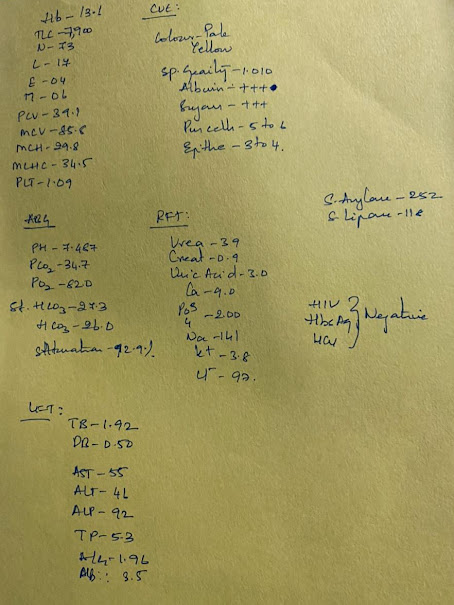
Investigations: 3/06/2022
Hemoglobin: 10.7 gm/dL (decreased)
Total Leucocyte Count: 34,500/ microlt (increased)
Absolute Leucocyte Count:
Neutrophils: 92
Lymphocytes: 4
Eosinophils: 0
Monocytes: 4
Basophils: 0
Packed cell volume: 29.7 (decreased)
Mean Corpuscular volume: 81.1
Mean Corpuscular hemoglobin: 29.2
Mean Corpuscular hemoglobin concentration: 36
RBC: 3.66 million/ microlt
Platelets: 2.5 lakh/ microlt
Blood smear: Normocytes Normochromic
Random blood sugar: 210 mg/dL (elevated)
Blood urea: 105 mg/dL (elevated)
Serum creatinine: 3.9 mg/dL (elevated)
Serum electrolytes:
Sodium: 135 mEq/L
Potassium: 4.1 mEq/L
Chloride: 98 mEq/L
Complete urine examination:
Pale yellow, clear urine
Albumin +
Sugar ++
Urinary electrolytes: Sodium- 238; K- 15.8; Cl- 302 mEq/day
Spot urine: Protein 17 mg/dL; Creatinine: 28 mg/dL; Ratio: 0.60
Liver function tests:
Total bilirubin: 1.09 mg/dL
Direct bilirubin: 0.19 mg/dL
SGOT: 14 IU/L
SGPT: 10 IU/L
Alkaline Phosphatase: 722 IU/L (elevated)
Total proteins: 5.3 gm/dL
Albumin: 2.97 gm/dL (decreased)
Albumin: Globulin ratio: 1.27
Pleural Tap was done
Wide bore needle used to do Pleural tap. (Image obtained from internet)
Pleural fluid had:
Sugar: 178 mg/dL
Protein: 3.8 gm/dL
LDH: 561
Serology: Negative
Ultrasound of abdomen report showed:
Simple Renal cortical Cysts
Right side 3mm Renal calculi in lower pole
Electrocardiogram:
Arterial Blood gas (ABG) report on 3/06/2022 at 6:17 pm:
pH - 7.13
pCO2 - 16.8
pO2 - 106
HCO3 - 5.4
St.HCO3 - 8.9
BEB - (-)23.3
BEecf - (-)22.3
TCO2 - 11.3
O2 saturation - 95.5
Investigations: 4/06/2022
Blood urea: 70 mg/dL (elevated)
Serum creatinine: 5 mg/dL (elevated)
Chest x ray:
Obliteration of right costochondral junction
ABG on 4/06/2022 at 7:25 pm:
pH - 7.22
pCO2 - 16.9
pO2 - 70.3
HCO3 - 6.8
St.HCO3 - 10.2
BEB - -19.5
BEecf - -19.7
TCO2 - 14.4
O2 saturation - 92.3
Investigations: 5/06/2022
Blood urea: 58 mg/dL (elevated)
Serum creatinine: 7.2 mg/dL (elevated)
ABG on 5/06/2022 at 1:56 pm
pH - 7.17
pCO2 - 17.0
pO2 - 101
HCO3 - 5.9
St.HCO3 - 9.1
BEB - -21.3
BEecf - -21.2
TCO2 - 13.0
O2 saturation - 95.3
Treatment given:
1) IV Fluids NS @ 50 mL/hr
2) Inj Augmentin 1.2 gm IV/TID
3) Inj Neomol 1 gm IV SOS
4) Inj Optineuron 1 Amp in 100 mL NS IV OD
5) Inj Lasix 40 mg IV BD
6) Inj PAN 40 mg IV OD
7) T. DOLO 650 mg PO QID
8) T. AZEE 500 mg PO OD
9) NEB with Duolin 8th hourly and Budecort 12th hourly
10) Inj Zofer 4mg IV SOS
Follow up:
On 5/6/2022
Patient developed Left side hemiplegia which worsened GCS
MRI brain revealed Acute ischemic stroke in the right middle cerebral artery territory (infarct)
Treatment added:
Tab Ecosprin 150mg OD
Tab Clopitab 75 mg OD
Tab Atocor 20 mg OD
On 6/6/2022 at 4:25 AM:
Patient became unresponsive with no cardiac activity
6 cycles of CPR with intubation and ROSC obtained. Patient was mechanically ventilated.
At 6:05 AM:
Patient again went into cardiac asystole
6 cycles of CPR failed to revive the patient
Declared dead at 6:35 am on 6/6/22
Cause of death:
Sepsis with Multi organ damage
Septic shock
Refractory metabolic acidosis



.jpeg)







Comments
Post a Comment