Case discussion on 28 year old Female with headache
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Short case
1701006128
Case discussion on 28 year old lady with headache
The case is of a 28 year old lady, resident of Valbapuram, Nakrekal, a farm labourer by occupation who was brought to casuality with:
Headache, giddiness and decreased responsiveness for a duration of 6 hours on 8/06/2022
Timeline of events and History of Presenting illness
Patient was a farm labourer by occupation
On 3/06/2022 at 4pm, she had an altercation with neighbours due to which her in laws started abusing her.
At 10:00 pm, as she was unable to cope with the situation, she impulsively drank rat poison. It was identified to be Zinc phosphide and she took about 12-14 gm.
She had 2 episodes of vomiting and abdominal pain and lost consciousness. There was no history of any seizures, shortness of breath, involuntary micturition and defecation.
She was brought to casuality by her husband. Was treated by giving Fresh frozen plasma transfusion due to deranged Prothrombin Time,APTT and INR.
Her ABG on 3/6/2022 showed slight acidosis with decreased carbonates. Hence she was managed with Inj of Sodium bicarbonate.
She was treated conservatively, improved on 4/06/2022 and was relieved by 6/06/2022 on which day she was discharged.
Present illness:
On 8/06/2022, in the afternoon, at around 12 pm, patient developed a headache. It was incidious in onset, progressive and generalized. It was associated with fever.
The fever was incidious in onset and progressive. Temperature was not documented but patient reports that it was high grade. No relieving factor. It was not associated with any chills or rigours, vomiting, abdominal pain, loose stools or burning micturition.
As the day progressed, she had loss of appetite, blurring of vision, difficulty in speech. Her husband reports altered behaviour and decreased responsiveness and brought her to the hospital at around 7 pm.
She had no history of seizures, shortness of breath, focal neurological deficit.
Her Glasgow coma score at the time of admission was:
Eye opening: 4
Verbal: 1
Motor: 6
Past history:
She had no similar complaints in the past.
No significant past psychiatric history
Not a known case of Hypertension, Diabetes mellitus, Asthma, Epilepsy, Coronary artery disease.
She had 2 Caesarean sections in the past due to no labour pains. No blood transfusions.
No significant drug history or substance abuse.
Personal history:
She takes a mixed diet
Appetite is reduced
Bowel and bladder are regular
Sleep is adequate
No allergies
No addictions
Family history:
No significant psychiatric illness in the family.
General Examination:
Patient is examined in a well lit room after obtaining informed consent. She is conscious, coherent and cooperative, well built and nourished. Supine position
On examination:
Pallor: Mild
Icterus, cyanosis, clubbing, koilonychia, generalized lymphadenopathy or edema are not observed.
No clubbing of nails observedPalmar creases seen
No icterus observed
Vitals:
At the time of admission:
Heart rate: 112 BPM (elevated)
Respiratory rate: 30 cycles per min (elevated)
Blood pressure: 120/80 mmHg
Temperature: 98.4°F
SPO2: 96% room air
RBS: 133 mg/dl
During examination:
Heart rate: 88 BPM
Respiratory rate: 20 cycles per min
Blood pressure: 110/70 mmHg
Temperature: 96.6°F
SPO2: 99% room air
RBS: 104 mg/dl
Systemic Examination:
Central Nervous System:
Higher mental functions:
Oriented to time,place,person
Memory : recent, remote intact
Speech: normal, understandable
No delusions or hallucinations
Cranial nerves:
1- not tested
2- binocular vision: normal
colour vision:normal
3,4,6- No restriction of movement of eye
5-normal( muscles of mastication+sensations of face) No jaw jerk
7-Normal, wrinking of forehead seen, able to blow up cheeks
8- Normal hearing, no nystagmus
9,10,11,12-normal. Gag reflex is normal.
Motor examination:
Bulk: Normal in all 4 limbs
Tone -Normal in all 4 limbs
Power
5/5 in both lowerlimbs
5/5 in upper limbs
Reflexes :
Biceps:2+
Triceps:2+
Supinator 2+
Knee: 3+
Ankle: 2+
Plantars: Flexion response
Sensory examination:
Crude touch, pain ,temp, fine touch, joint position, proprioception are normal in all dermatomes in upper limbs and lower limbs
Cerebellum examination:
Able to do finger nose test.
No dysdiadokinesia
No rebound phenomenon
Autonomic Nervous System:
No postural hypotension
No bladder and bowel incontinence
No sweating abnormalities
Meningeal signs:
No meningal signs like Brudzinski or Kernig sign were positive
Gait:
Normal
Goes to bathroom by herself
Other systems examination:
CVS: S1 S2+ no murmurs heard.
Respiratory system- Bilateral air entry+ ,normal vesicular breath sounds-heard.
Abdominal: Soft, non tender, no distension, umbilicus is central and inverted,no scars, no sinuses, hernial orifices free.
Provisional diagnosis:
Headache under evaluation (secondary to Migraine)
K/c/o Zinc phosphide poisoning
Management:
Investigations:
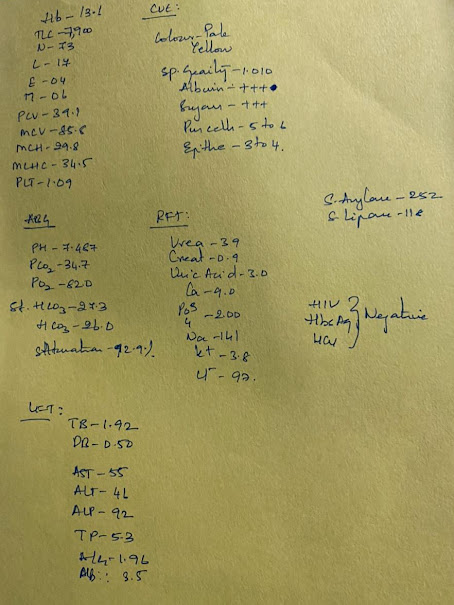
Hemoglobin: 10.9 gm/dL (decreased)
Total Leucocyte Count: 6500/ microlt
Absolute Leucocyte Count:
Neutrophils: 80
Lymphocytes: 10
Eosinophils: 1
Red Blood Cell count: 4.35 cells/microlt
Platelets: 1.25 lakh/ microlt
Blood urea: 17 mg/dL
Serum creatinine: 0.8 mg/dL
Complete Urine examination:
Clear
Albumin: Negative
Pus cells: 2-3
Epithelial cells: 2-3
Serum electrolytes:
Sodium: 140 mEq/L
Potassium: 3.9 mEq/L
Chloride: 101 mEq/L
Phosphorus: 2.2 gm/dL
Prothrombin time: 16 sec
Activated thromboplastin time: 31 sec
INR: 1.11
Electrocardiogram:
MRI showed no abnormality in brain, orbit or paranasal sinuses.
Psychiatric referral notes:
Mental status examination:
General appearance and behaviour: Patient is lying on bed comfortably, responding to oral commands.
Speech: Normal in tone, volume and relevance
Thought: No abnormality detected
Mood: Pleasant
Affect: Euthymic
Perception: No abnormality detected
Impression: Impulsive Self harm
Treatment: Counselling of patient and attenders
Treatment:
1) Tab Naproxen 250 mg PO/BD
2) Tab Neurobion Forte PO/BD
3) Tab Pantop 40 mg PO/OD
4) Tab Amitriptyline 10 mg PO/SOS
5) IV fluid NS @ 100 ml/hr
6) Vitals monitoring












Comments
Post a Comment