This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome.
Neha Tipparaju
Roll no. 100
Case of a 75 year old lady brought in an unresponsive state
My case is of a 75 year old lady, a homemaker in Miryalguda, who was brought to casuality in an unresponsive state with no recordable blood pressure and no pulse. SPO2 35% on 15 liters of O2.
CPR was started according to 2020 American Heart Association guidelines.
Patient was intubated with 7.5 cm Endotracheal Tube and bilateral air entry checked cycles of CPR were done with 1 milligram adrenaline after each cycle
Return of Spontaneous Circulation was obtained after 6 cycles.
Timeline of events and History of Presenting Illness:
Patient lived a normal life, taking turns residing with her 4 sons.
20 years back, Patient had an episode of chest pain and palpitations. She was taken to a private hospital and diagnosed to have Myocardial Infarction due to coronary occlusion and a Percutaneous Coronary Angioplasty was done with a stent placed. She was also diagnosed with Diabetes Mellitus, Hypertension and Obstructive Sleep Apnea. She has been on regular medication since then.
In 2017, she suddenly developed shortness of breath, drowsiness and pedal edema. She was diagnosed to have Type 2 respiratory failure due to her OSA.
In the private hospital,
2D echo showed : mild concentric LVH, normal LV function and Grade 3 diastolic dysfunction.
CT pulmonary angiography showed Pleural effusion and Ground glass opacities.
Sleep studies were done and the patient was advised BiPAP which she used every night.
Since then, she has been taking her medication regularly and also monitoring her weight, blood sugar levels and her blood pressure.
Atorvastatin + Clopidogrel
Metformin
In December, 2021 she had recurrent episodes of shortness of breathlessness, early in the morning which was sudden in onset, relieved on lying down, occuring every 10 days. She was taken to a local hospital during one of these episodes and was advised nebulization of the following drugs when the attack repeats:
1 month back, The patient stopped using BiPAP due to technical difficulty and since then she was said to have excessive daytime sleepiness.
On the morning of 29/3/2022, Patient awoke from sleep and was continuing her activities when she suddenly developed shortness of breath of Grade 4. She was given nebulization at home but did not improve and so taken to a local doctor who found her blood pressure to be 230/110 mmHg. He administered an injection of Labetalol. The patient was on her way to Hyderabad in an ambulance when she became unresponsive and went into cardiac arrest. She was then brought to our hospital where she was resusitated.
Post CPR vitals:
Afebrile
BP 170/100
PR 110 BPM
CVS S1,S2 +
RS BAE+, Decreased air entry in Lt mammary area
Patient has not regained consciousness. She has episodes of seizures where she had eye opening and clonic movements.
Personal history:
The patient is a pure vegetarian. Her appetite, before the event was normal and bowel and bladder were regular. She had excessive daytime sleepiness. No allergies and addictions.
Family history: Not significant
General Examination:
Patient is examined in a well lit room, in supine position. She is not conscious and is seen to be on ventilatory support. Sedated and paralysed.
On examination no signs like pallor, icterus, cyanosis, clubbing or generalized lymphadenopathy were observed. Pedal edema with discolouration of feet is seen.
Vitals: BP: 130/70 mmHg ;
Pulse Rate: 75 BPM
Afebrile
fiO2: 100%
Tidal volume: 450 mL
CNS: myoclonus
CVS: JVP NORMAL, Apex beat 5th Intercostal space Mid Clavicular line s1s2 +
RS: BAE + , decreased air entry on right side IMA, IAA
P/A: soft, non tender , BS +
Provisional diagnosis:
Acute type 2 respiratory failure secondary to Obstructive Sleep Apnea and Hypertension following a Cardiac arrest.
Investigations:
Blood group typing: O POSITIVE
RBS: 211mg/dl
HbA1c : 6.8%
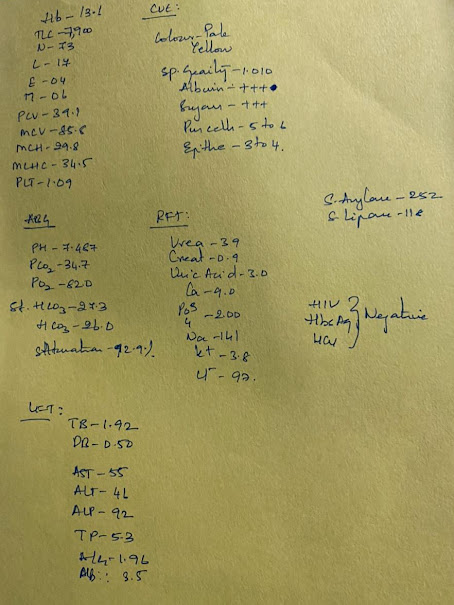
Renal function test:
Blood Urea: 49mg/dl
S. Creatinine: 1.9mg/dl
Na 142
K 4.7
Cl 98
Hemogram
HB 8.5
TLC 13,600
MCV 85.9
PCV 27.4
MCH 26.6
MCHC 31
PLT 2.0
P.S NORMOCYTIC, NORMOCHROMIC with neutrophilic leucocytosis
Serum iron : 45ug/dl
ABG post CPR fio2 100%
pH 6.88
PCo2 107
PaO2 77.4
HCO3 11.8
SpO2 82.5
Metabolic and Respiratory Acidosis
ABG day 0 evening fio2 80%
pH 7.46
PCo2 32.8
PaO2 146
HCO3 23.1
SpO2 98.5
ABG day 1 morning fio2 50%
pH 7.43
PCo2 31.9
PaO2 95.3
HCO3 22.6
SpO2 96.8
ABG day 1 morning fio2 40%
pH 7.4
PCo2 31.9
PaO2 80
HCO3 21.5
SpO2 94.7
LFT
TB 0.57
DB 0.16
AST 148
ALT 123
ALP 180
TP 4.7
ALB 2.2
CUE
ALB ++
Sugars nil
Pus cells 4-5
Epithelial cells 1-2
Chest x ray:
Expiratory field, PA view showing cardiomegaly and prominent bronchiovascular , hazziness, effusion
30/3/22
ECG:
Post CPR:
2D echo
Concentric LVH
Sclerotic AV
EF 58%
RVSP 35 mmHg
Diastolic dysfunction +
Treatment
Ventilatory support
IVF NS/RL @50ML/HR
Inj. Pan 40 mg IV OD
Inj. Zofer 4 mg IV SOS
Inj. Midazolem titrate B/W 0.1 - 3 mg/Kg
Inj. Atracurium @ 0.8ml/hr (10mcq/hr)
Inj. Levipil 1gm IV STAT
Inj. Levipil 500 mg IV TID
Inj. Clexane 60mg sc OD
RT feeds milk+protein 100ml, water 100ml q4hrly
Propped up position
Air bed with position change 2nd hourly
Temperature: 102.1°F
Pulse rate: 118
Respiratory rate: 12 bpm
SpO2: 98
GRBS: 146 mg/dl


























Comments
Post a Comment